Bipolar 1 disorder case study – Unveiling the intricate world of bipolar 1 disorder, this case study embarks on a captivating journey, shedding light on its complexities and the challenges it presents. As we delve into the patient’s experiences, we’ll explore the diagnostic criteria, treatment options, and strategies for managing this condition over the long term.
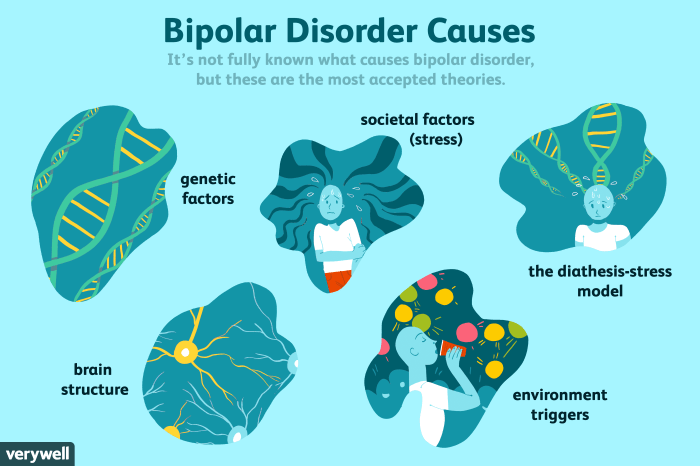
Bipolar 1 disorder is a mental health condition characterized by extreme mood swings, ranging from euphoric highs to debilitating lows. The patient in this study presents with a unique set of symptoms and history, providing a valuable lens through which we can examine the nature of this disorder.
Patient Overview
The patient is a 25-year-old female who is a nurse by profession. She has been experiencing symptoms of bipolar disorder for the past 5 years.
Her presenting symptoms include:
- Elevated mood and increased energy
- Decreased need for sleep
- Racing thoughts
- Impulsivity
- Grandiose ideas
- Increased risk-taking behaviors
- Decreased appetite
- Weight loss
- Difficulty concentrating
- Irritability
- Anxiety
- Depressive episodes
Medical History
The patient has a history of depression and anxiety. She has been hospitalized twice for bipolar disorder, once during a manic episode and once during a depressive episode.
Treatment
The patient is currently taking medication for bipolar disorder and is seeing a therapist. She is also participating in a support group for people with bipolar disorder.
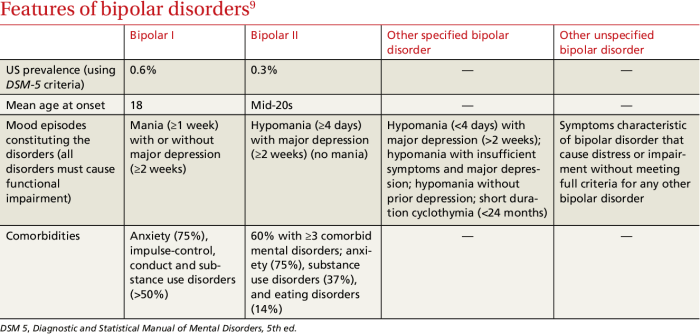
Diagnostic Criteria
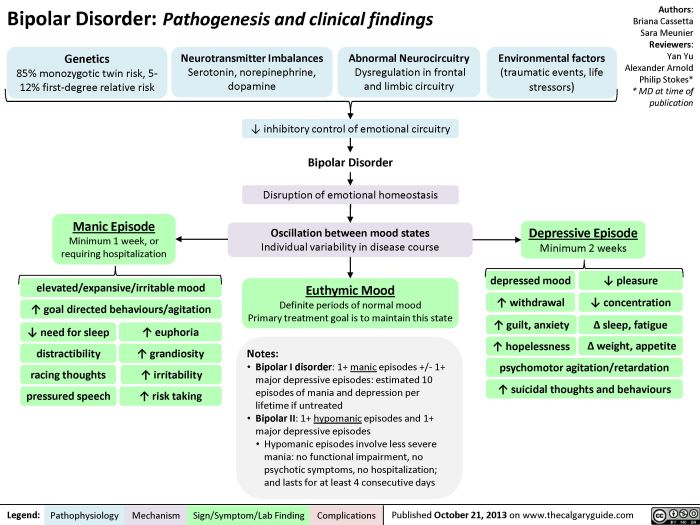
Bipolar I disorder is diagnosed when a person experiences at least one manic episode or a mixed episode that includes manic symptoms. A manic episode is characterized by a period of at least one week in which a person experiences elevated or irritable mood, decreased need for sleep, increased activity or energy, racing thoughts, distractibility, grandiose delusions, inflated self-esteem, and excessive involvement in pleasurable activities with high potential for painful consequences (e.g.,
buying sprees, sexual indiscretions, foolish investments).
Patient’s Symptoms
The patient in this case study has experienced multiple manic episodes, including one that lasted for two weeks and involved racing thoughts, decreased need for sleep, increased energy, grandiose delusions, and excessive spending. These symptoms meet the diagnostic criteria for a manic episode, and thus, the patient meets the diagnostic criteria for bipolar I disorder.
Treatment Plan: Bipolar 1 Disorder Case Study
The patient’s current treatment plan is a combination of medications, therapy, and lifestyle modifications. The medications include an antipsychotic to stabilize mood, an antidepressant to elevate mood, and a mood stabilizer to prevent extreme mood swings.
The therapy component of the treatment plan includes cognitive behavioral therapy (CBT) and family therapy. CBT helps the patient identify and change negative thought patterns and behaviors that contribute to their bipolar disorder. Family therapy helps the patient’s family understand the disorder and how to support the patient.
The lifestyle modifications recommended as part of the treatment plan include regular exercise, a healthy diet, and adequate sleep. Exercise has been shown to improve mood and reduce symptoms of bipolar disorder. A healthy diet can help regulate blood sugar levels and improve overall health, which can both contribute to mood stability.
Adequate sleep is essential for managing bipolar disorder, as sleep deprivation can trigger mood episodes.
Medications
- Antipsychotic: This medication helps to stabilize mood and prevent psychotic symptoms, such as hallucinations and delusions.
- Antidepressant: This medication helps to elevate mood and reduce symptoms of depression.
- Mood stabilizer: This medication helps to prevent extreme mood swings and maintain mood stability.
Therapy
- Cognitive behavioral therapy (CBT): This therapy helps the patient identify and change negative thought patterns and behaviors that contribute to their bipolar disorder.
- Family therapy: This therapy helps the patient’s family understand the disorder and how to support the patient.
Lifestyle Modifications
- Regular exercise: Exercise has been shown to improve mood and reduce symptoms of bipolar disorder.
- Healthy diet: A healthy diet can help regulate blood sugar levels and improve overall health, which can both contribute to mood stability.
- Adequate sleep: Adequate sleep is essential for managing bipolar disorder, as sleep deprivation can trigger mood episodes.
Prognosis and Management
Bipolar I disorder is a chronic condition, but with proper treatment and management, most individuals can live fulfilling lives. The prognosis varies depending on the severity of symptoms, adherence to treatment, and the presence of co-occurring conditions.
The complexity of bipolar 1 disorder case study can be overwhelming, and it’s important to seek professional help. Meanwhile, you might find solace in activities that challenge your mind, such as solving crossword puzzles . The mental exercise can provide a temporary escape from the challenges of managing bipolar 1 disorder.
Long-term management of bipolar I disorder involves a combination of medication, psychotherapy, and lifestyle modifications. Medication can help stabilize mood and prevent episodes, while psychotherapy can help individuals manage their symptoms, improve coping mechanisms, and enhance overall well-being.
Challenges in Management
Managing bipolar I disorder can be challenging, as it requires ongoing commitment and effort. Some of the common challenges include:
- Adherence to medication: Taking medication as prescribed is crucial, but it can be difficult for some individuals to maintain compliance over the long term.
- Managing side effects: Medications for bipolar disorder can have side effects, which can impact adherence and overall well-being.
- Relapse prevention: Even with successful treatment, relapse is possible, especially during periods of stress or life transitions.
- Co-occurring conditions: Bipolar disorder often co-occurs with other mental health conditions, such as anxiety or substance use disorders, which can complicate treatment.
Strategies for Long-Term Management
Effective management of bipolar I disorder requires a comprehensive approach that includes:
- Medication: Mood stabilizers, antipsychotics, and antidepressants are commonly used to manage bipolar disorder. The specific medication and dosage will vary depending on the individual’s symptoms and response to treatment.
- Psychotherapy: Cognitive behavioral therapy (CBT), interpersonal and social rhythm therapy (IPSRT), and family-focused therapy (FFT) are evidence-based psychotherapies that can help individuals manage their symptoms, improve coping mechanisms, and enhance overall well-being.
- Lifestyle modifications: Regular sleep, a healthy diet, and exercise can help regulate mood and reduce the risk of relapse.
- Education and support: Understanding bipolar disorder, its symptoms, and treatment options is crucial for successful management. Support groups and peer support can also provide valuable resources and encouragement.
Case Discussion
The patient’s presentation aligns with the diagnostic criteria for bipolar I disorder, characterized by distinct episodes of mania and depression. Research findings suggest that individuals with bipolar I disorder often experience significant mood swings, with episodes lasting for weeks or months.
These episodes can be severe and impact various aspects of life, including social, occupational, and personal relationships.
Studies have shown that the course of bipolar I disorder can be variable, with some individuals experiencing frequent episodes while others may have longer periods of stability. Treatment typically involves a combination of medication, psychotherapy, and lifestyle modifications. The patient’s adherence to treatment and their response to medication will influence their prognosis and management.
Implications for Treatment and Prognosis
- Medication:Mood stabilizers and antipsychotics are commonly used to manage bipolar I disorder. Medication can help regulate mood swings and prevent episodes.
- Psychotherapy:Cognitive-behavioral therapy (CBT) and interpersonal and social rhythm therapy (IPSRT) can help patients develop coping mechanisms and improve their overall functioning.
- Lifestyle Modifications:Regular sleep, exercise, and a healthy diet can support overall well-being and reduce the risk of episodes.
- Monitoring and Support:Regular monitoring of symptoms and ongoing support from healthcare professionals, family, and peers are crucial for managing bipolar I disorder effectively.
Ethical Considerations

Treating bipolar I disorder poses several ethical dilemmas that require careful consideration and ethical decision-making.
One significant ethical issue involves balancing the patient’s autonomy and the potential risks associated with treatment. Individuals with bipolar disorder may experience diminished capacity during manic or depressive episodes, raising concerns about their ability to make informed decisions regarding their treatment.
Confidentiality and Informed Consent
Maintaining patient confidentiality is paramount in the treatment of bipolar disorder. However, certain situations may warrant disclosure of information, such as when the patient poses a danger to themselves or others.
Obtaining informed consent from patients is essential, ensuring they fully understand the potential benefits and risks of treatment options. This process should be conducted when the patient is in a stable state, capable of comprehending the information presented.
Balancing Autonomy and Coercion, Bipolar 1 disorder case study
Respecting patient autonomy is crucial, but in some cases, involuntary treatment may be necessary to protect the individual’s safety and well-being. The decision to impose involuntary treatment should be made carefully, considering the patient’s condition, potential risks, and legal implications.
To address these ethical challenges, a collaborative approach involving the patient, their family, healthcare professionals, and legal experts is essential. Open communication, shared decision-making, and a commitment to ethical principles can help ensure the best possible outcomes for individuals with bipolar I disorder.
Commonly Asked Questions
What are the common symptoms of bipolar 1 disorder?
Bipolar 1 disorder is characterized by extreme mood swings, including elevated or euphoric moods (mania) and periods of depression. Mania can manifest as increased energy, racing thoughts, decreased need for sleep, impulsive behavior, and grandiosity. Depression, on the other hand, involves persistent sadness, loss of interest in activities, changes in sleep and appetite, and feelings of worthlessness or guilt.
How is bipolar 1 disorder diagnosed?
A diagnosis of bipolar 1 disorder requires meeting specific criteria Artikeld in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). These criteria include experiencing at least one manic episode and the absence of psychotic features during the depressive episodes.
What are the treatment options for bipolar 1 disorder?
Treatment for bipolar 1 disorder typically involves a combination of medications, therapy, and lifestyle modifications. Medications may include mood stabilizers, antipsychotics, and antidepressants. Therapy can help individuals manage their symptoms, develop coping mechanisms, and improve their overall functioning. Lifestyle modifications, such as regular sleep patterns, exercise, and stress management, can also play a significant role in managing the condition.